Antimicrobial resistance has been said to be the next biggest threat after the COVID-19 pandemic. But what is antimicrobial resistance? How does it affect us? What can we do to stop it? And what should we be doing? This RI Expert Briefing seeks to answer these questions.
What are antimicrobials?
Antimicrobials are medicines used to prevent and treat infections in humans, animals and plants, by destroying or inhibiting the growth of microorganisms.1 Examples of antimicrobials include antibiotics, antivirals, antifungals and antiparasitics.
What is antimicrobial resistance (AMR)?
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites mutate and change over time to the point that they become immune to medicines and no longer respond to them. Through natural selection, antibiotics remove drug-sensitive competitors, whilst drug-resistant bacteria continue to reproduce.
This makes infections much more difficult to treat and increases the risks of disease spread, severe illness and death. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.2
what are the main causes of the AMR crisis?
Overuse
One of the main drivers of AMR has been the overuse of antibiotics. Studies have shown a direct link between antibiotic consumption and the development of resistant bacteria strains.3 Despite warnings of the dangers of overuse, antibiotics are over-prescribed worldwide, and in some countries, such as Romania and Greece4, antibiotics are available online and over the counter without a prescription.5
The lack of regulation surrounding the usage of easily accessible and cheap antibiotics promotes overuse, and thus increases the likelihood of developing resistance.6
Inappropriate Prescribing
In addition to overuse, incorrectly prescribed antibiotics can also contribute to the increase of resistant microorganisms. 30% to 60% of antibiotics used in intensive care units (ICUs) in America were deemed unnecessary, inappropriate or suboptimal.7
It has also been shown that in 30%–50% of cases the treatment indication, choice of agent, or duration of therapy were incorrectly prescribed. Incorrectly prescribed antibiotics and suboptimal concentrations can lead to reduced therapeutic benefit exposing patients to complications of antibiotic therapy and promote the development of antibiotic resistance.
Extensive Agricultural Use
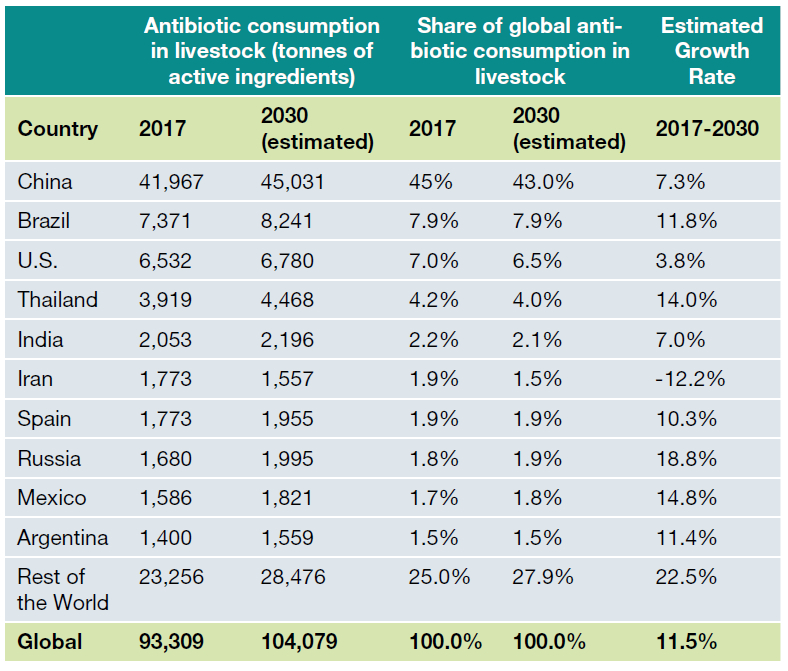
Worldwide it is estimated that 73% of all antibiotics are used in livestock, with consumption expected to rise 67% by 2030. Whilst the global usage of antimicrobials varies depending on each country, the top 10 veterinary antimicrobial consumer countries in 2017 (table 1) accounted for 75% of global antimicrobials used in animal husbandry. China was the largest consumer of veterinary antimicrobials, accounting for 45% of global use, and is projected to remain the largest consumer in 2030 (43%).8
Antibiotics are used globally to promote growth in livestock and prevent disease spread as animals are kept in poor conditions where disease can spread easily. This is said to improve the overall health of the animals, their size, producing larger yields and higher-quality products. Whilst the use of antibiotics for growth promotion has been banned throughout the EU since 2006, it is still used widely for health purposes.9 As of 2016, the EU member countries with the highest usage of antibiotics in livestock were Cyprus, Spain and Italy.10
Alarmingly, resistant bacteria in livestock was found to reach consumers through meat products when ingested, causing infections in humans that may lead to adverse health consequences. Farmers were found to be at risk of direct transfer of resistant bacteria as high rates of antibiotic resistance were discovered in the intestinal flora of both farm animals and farmers.11
The use of antibiotics in livestock also has an impact on the environment, as these are excreted in urine and stool, and then widely distributed through fertilisers, and groundwater. This means that even fruits and vegetables can be exposed to drugresistant bacteria as they are usually grown using animal fertilisers which may contain antibiotics.
Additionally, another way of distributing bacteria is through water. Large amounts of antibiotics are released into municipal wastewater, either from human metabolism or disposal of unused antibiotics, leading to high concentrations of antibiotic resistant bacteria in wastewater treatment plants.12
Availability of Few New Antibiotics
The development of new antibiotics by pharmaceutical companies has stalled in recent years due to both economic and regulatory obstacles. Additionally, mergers between pharmaceutical companies have reduced the number of research teams, whilst on the academic front, antibiotic research has been scaled back as a result of funding cuts. As of 2020, 74 antimicrobial drugs were in clinical development stages, of which only 10 were either approved or in Phase IV clinical trials.13
A 2017 analysis estimated the cost of developing an antibiotic at around US$1.5 billion, with an average revenue of US$46 million per year.14 Additionally, the net present value (NPV) of a new antibiotic is found to be only about US$50 million, compared to approximately US$1 billion for a drug used to treat a neuromuscular disease.
With the combination of their low cost and short period usage, antibiotics are not deemed to be as profitable as drugs for chronic conditions. As physicians are advised against prescribing new antibiotics where possible, this leads to a lower return on investment as a result of the reduced usage. Hence, it is no longer considered to be an economically wise investment for the pharmaceutical industry to develop new antibiotics.
When new antimicrobial agents are found and used, the emergence of resistance is practically guaranteed. As bacterial evolution is uncertain, the timeline for the development of resistance is unpredictable. A pharmaceutical company that invests millions of dollars in the development of new antibiotic drugs may discover that their profits are prematurely reduced when drug resistance is developed.15
why is amr a concern?
Resistance to antimicrobials does not only affect one industry but rather could impact and destabilise many industries, predominantly; health services, manufacturers of antibiotics, pharmaceutical companies, animal health companies, farmers, and the food industry.
In 2019, then Chief Medical Officer for England, Sally Davies, issued a warning to the head of the United Nations saying that if no action is taken on antimicrobial resistance, 10 million people worldwide could die each year by 2050.16 It is estimated that the AMR crisis could lead annual costs ranging from $300 billion to more than $1 trillion globally by 205017 and lead to a global GDP reduction of 3%.18
With the spread of drug-resistant pathogens and ineffective antibiotics, the threat to our ability to treat common infections increases. The cost of AMR to national economies and their health systems is substantial as it affects patients through prolonged hospital stays and the need for more expensive and intensive care. This can result in medical procedures, such
as surgery, cancer chemotherapy, and organ transplantation, becoming riskier.
This is particularly alarming as countries with high rates of malaria, HIV and Tuberculosis (TB), which require antibiotic treatment, are likely to predominantly suffer as resistance to current treatments increases. If drug resistance to these diseases is not tackled the devastating impacts of HIV and TB, which are already seen in many of the poorest parts of the world, will likely get worse. Moreover, drug-resistant malaria could constrain the economic progress achieved by some countries in Asia, leading to a negative impact on the large export sectors in these countries.19
amr and covid-19
The COVID-19 pandemic has had an impact on everyone’s lives, although affecting every country and industry differently. Since the emergence of COVID-19, data has shown an increase in antibiotic use, even though most of the initial illnesses being treated have been from the COVID-19 viral infection. The resulting increased exposure to healthcare settings and invasive procedures, along with expanded antibiotic use, amplifies the opportunity for resistant pathogens to emerge and spread. Whilst antibiotics can’t fight the COVID-19 virus, nearly 15% of people hospitalised with COVID-19 went on to develop bacterial pneumonias, some of which are already resistant to existing antibiotics.20
It is as yet unknown the extent to which the pandemic is directly impacting overall levels of AMR, but a review of data from Asia shows that over 70% of COVID-19 patients received antimicrobial treatment, whilst only 10% had bacterial or fungal infections.21
In developing countries, such as India, where poor hygieneand inadequate sanitation systems lead to high levels of infectious diseases, the fight to tackle AMR has taken a backseat during the pandemic. The antibiotic overuse in these countries has left health officials with fears that AMR will accelerate following the pandemic.22
how are different industries responding?
Interagency Coordination Group on Antimicrobial Resistance (IAGC)
In April 2019, the IAGC issued a report to the Secretary- General of the United Nations detailing five key recommendations to tackle the AMR crisis globally (fig.1)23 The report details actions required from Member States, researchers, civil society groups, governments and investors to tackle this crisis and achieve the Sustainable Development Goals. Factors such as inadequate access to clean water, sanitation and hygiene; poor disease prevention; lack of access to affordable medication; and poor food safety and waste management systems are all contributing to the emergence and acceleration of drug-resistant pathogens.
Pharmaceutical Industry
In July 2020, the International Federation of Pharmaceutical Manufacturers and Associations announced the AMR Action Fund. The antimicrobial-resistance initiative involves 24 companies, including pharmaceutical giants Pfizer and GSK. It aims to bring between 2-4 new antibiotics to patients by 2030, and has so far committed nearly $1 billion to support the research required in order to achieve this goal.24
Government Action
In May 2020, the European Commission announced the launch of the Farm to Fork strategy, designed to make food systems sustainable. Amongst its objectives is to reduce overall EU sales of antimicrobials for farmed animals and in aquaculture by 50% by 2030.25 Other regulatory measures in the EU include a pending ban from 2022 on antibiotic use in animals without authorisation from a vet.
In the U.S. the proposed Pasteur Act aims to support the development of new antibiotics and promote the appropriate use of existing ones, thus limiting the increase and spread of resistant infections.26 In 2016, China announced a ban on the use of Colistin as a growth promoter, and published a national action plan for dealing with antimicrobial resistance; in July 2020, the ban on the use of growth promoters in animal feed went into effect.27 Other countries, including Brazil, Japan and India, have since followed China and also banned Colistin as a growth promoter.
Food Industry
In March 2021, Yum! Brands, the parent company of KFC, Taco Bell and other fast-food chains agreed to publish a comprehensive report on the systemic effects of antimicrobial resistance (AMR) in its supply chain by the end of 2021, making it the first company to disclose this information. In 2018, McDonald’s announced a policy to reduce the overall use of antibiotics important to human health across 85% of their global beef supply chain.28
investor initiatives
Several non-profit organisations have launched initiatives and collaborative engagements to tackle the AMR crisis. Engagements are run with food companies, pharmaceutical companies, and protein producers.
Farm Animal Investment Risk & Return (FAIRR) Initiative
The FAIRR Initiative is a collaborative investor network that raises awareness of the environmental, social and governance (ESG) risks and opportunities brought about by intensive animal agriculture. FAIRR helps investors to identify and prioritise these factors through research and collaborative engagements on various topics, including AMR.29
Access to Medicine Foundation
The Access to Medicine Foundation has been working to stimulate and guide the pharmaceutical industry to do more for people living in low and middle-income countries for more than ten years.
The Foundation issues the Access to Medicine Index which ranks 20 of the world’s largest pharmaceutical companies based on three areas of behaviour linked to access: Governance of Access, Research & Development, and Product Delivery.
In 2018 the foundation also released The Antimicrobial Resistance Benchmark, which is the first report to compare what pharmaceutical companies are doing to bring antimicrobial resistance under control.
Business Benchmark on Farm Animal Welfare (BBFAW)
The Business Benchmark on Farm Animal Welfare (BBFAW) is a non-profit organisation, which measures and reports on farm animal welfare management (which includes antibiotic usage), policy commitment, performance and disclosure in food companies.
what is edentree's approach?
As part of our investment strategy within all EdenTree screened funds we do not invest in companies with more than 10% revenue from intensive animal farming, including aquaculture.
Furthermore, we support the development of new antibiotics by investing in pharmaceutical companies across all our portfolios, and we engage with these companies where appropriate. Amongst our engagement topics are; AMR, affordable product pricing, product safety, clinical trial data, product pipeline and lobbying.
We are signatories to all three investor initiatives mentioned above, and engage with them where appropriate depending on our holdings. We have supported the FAIRR initiative on antibiotic resistance and have signed investor letters on the topic of ‘use of antibiotics in the supply chain’.
We have also engaged in the past with supermarkets and food retailers on various topics regarding health and nutrition, including AMR.
In the year of pandemic, the critical importance of new discovery drugs has never been more urgent and obvious. As well as continuing to engage with the debate on AMR, we will press companies to commit research & development capital to the development of a new generation of antibiotics, without which once lethal diseases such as TB may once again become predator killers.
sources
1 https://www.merriam-webster.com/dictionary/antimicrobial
2 https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/pdf/ptj4004277.pdf
4 https://www.combacte.com/news/7-of-antibiotics-in-the-eu-are-takenwithout-a-prescription/
5 https://www.who.int/bulletin/volumes/98/7/19-242370/en/
6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4165128/pdf/fpubh-02-00145.pdf
7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4281952/pdf/13054_2014_Article_480.pdf
8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766021/pdf/antibiotics-09-00918.pdf
9 https://www.saveourantibiotics.org/the-issue/antibiotic-overuse-in-livestockfarming/
10 https://www.europeandatajournalism.eu/eng/News/Data-news/Fewerantibiotics-in-European-livestock-farming
11 https://pubmed.ncbi.nlm.nih.gov/23403172/
12 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4768623/pdf/ypgh-109-309.pdf
13 https://accesstomedicinefoundation.org/amr-benchmark/results/pipelinewhich-companies-are-developing-new-treatments-for-the-most-threateningbacteria-and-fungi
14 https://www.nature.com/articles/d41586-020-02884-3
15 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3654619/pdf/viru-4-185.pdf
16 https://www.nature.com/articles/d41586-019-01409-x
17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6929930/pdf/idr-12-3903.pdf
18 https://assets.kpmg/content/dam/kpmg/pdf/2014/12/amr-report-final.pdf
19 AMR-review: https://bit.ly/3xbQCy4
20 https://www.nature.com/articles/d41586-020-02418-x
21 https://www.bmj.com/content/bmj/369/bmj.m1983.full.pdf
22 https://www.ft.com/content/0a5d3051-b804-4485-a7a3-e144a712ebf4
23 https://www.who.int/antimicrobial-resistance/interagency-coordinationgroup/IACG_final_report_EN.pdf?ua=1
24 EIB: https://bit.ly/2RUfqdR
25 https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:52020DC0381
26 Antibiotic resistance: how to tackle a public health crisis | Financial Times (ft.com)
27 https://www.nature.com/articles/d41586-020-02889-y
28 https://corporate.mcdonalds.com/corpmcd/en-us/our-stories/article/ourstories.beef_antibiotics.html